This article reviews group psychotherapy research published within the past 30 years, predominantly focusing on outcomes of group treatments for patients with various mental disorders. Additionally, meta-analyses on the efficacy of group treatments for patients with cancer or chronic pain are summarized. Results strongly support the use of group therapy and demonstrate outcomes equivalent to those of individual psychotherapy. The research also appears to emphasize the effect of feedback on outcomes in group treatments and an association between treatment outcomes and group cohesion and alliance. Other promising developments in the field of group therapy are discussed.
Because of the long tradition of research on group psychotherapy and the growing importance of evidence-based standards, a large number of randomized controlled studies (RCTs) on the efficacy of group psychotherapy are available. Since 2013, numerous meta-analyses have been published through international cooperation among colleagues from the United States (Gary Burlingame, Brigham Young University), Germany (Bernhard Strauss and Jenny Rosendahl, University of Jena), Canada (Giorgio Tasca, University of Ottawa), and Italy (Gianluca Lo Coco, University of Palermo). In a joint effort, 11 meta-analyses have been conducted, including 329 RCTs (370 comparisons between group therapy and various control groups) and more than 27,000 patients. In the new edition of the Handbook (2), the evidence on group therapy is summarized according to the highest level of evidence-based research, allowing for specification of direction and strength of differences between treatment conditions (7), calculation of overall effect, and estimation of heterogeneity on individual study effects (8). Figure 2 provides an overview of the disorder-specific findings of the individual meta-analyses.
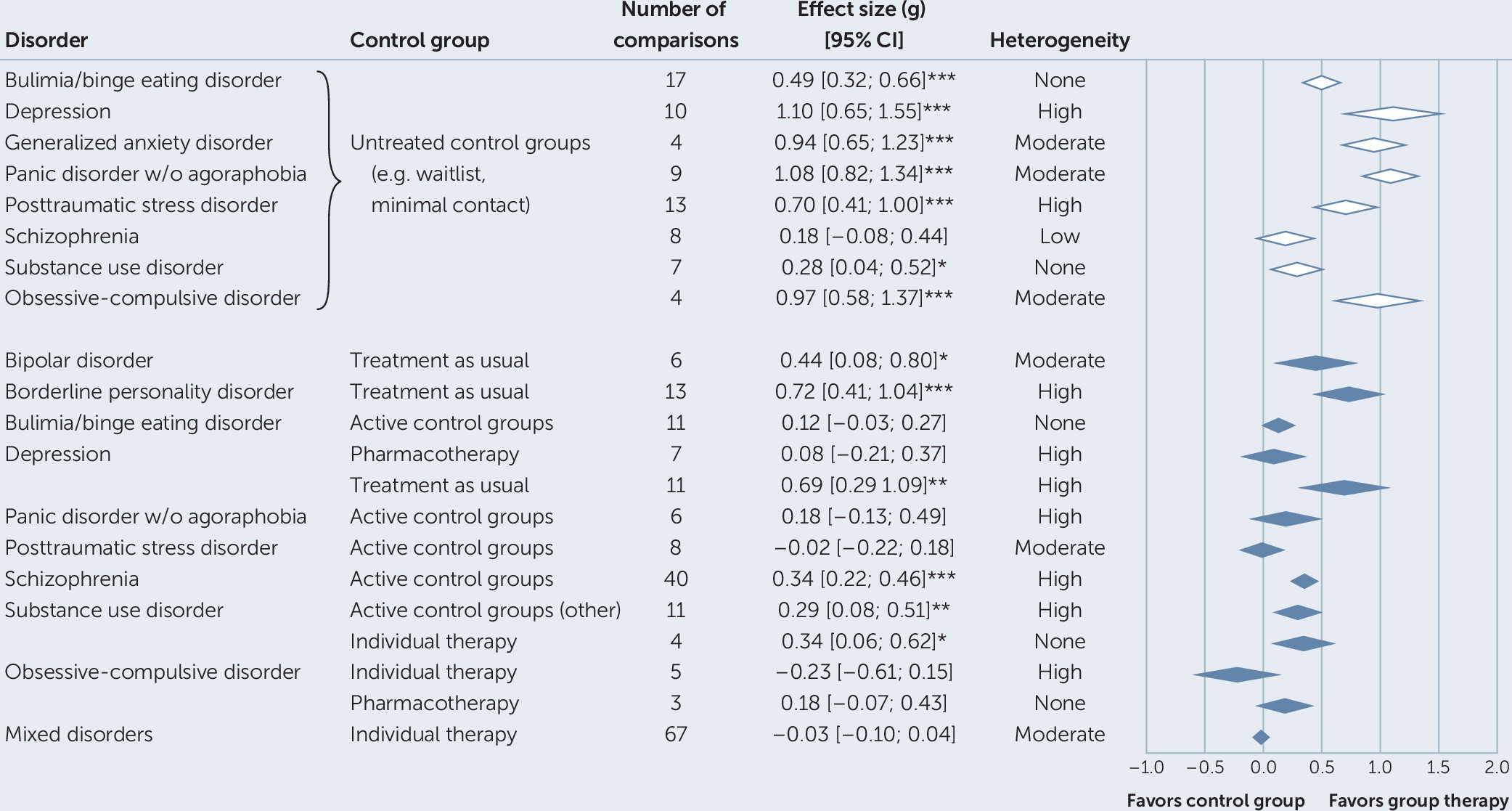
To date, 11 different meta-analytic summaries (9–19) have been based on RCTs examining the efficacy of group psychotherapy for patients with mental disorders. In comparison to untreated control groups (e.g., waitlist control groups, minimal contact conditions), group psychotherapy has demonstrated large effects on the reduction of disorder-specific symptoms associated with anxiety, obsessive-compulsive disorders, and depression. For eating disorders (e.g., bulimia, binge eating disorder) and posttraumatic stress disorder (PTSD), medium effects have been found (12, 14). Additionally, small effects have been shown for substance use disorders and schizophrenia (16, 17).
Comparisons to active treatment conditions (e.g., individual psychotherapy, pharmacotherapy, inpatient or outpatient treatment as usual) have yielded a more complex picture. Compared with inpatient or outpatient treatment as usual, group psychotherapy has demonstrated significant advantages with medium to large effect sizes on disorder-specific symptoms for patients with depression, bipolar disorder, and borderline personality disorder (15, 19). Specific comparison with pharmacotherapy (11, 19) has been available only in the context of obsessive-compulsive disorders and depression, with no significant differences found.
In comparisons between group psychotherapy and individual psychotherapy, disorder-specific findings have been identified for obsessive-compulsive disorders (no differences) and substance-induced disorders (small effect in favor of group therapy). In a meta-analytic summary comparing group and individual therapy across various disorders (10), 46 studies with equivalent treatments (treatment protocol, patients, dosage) across formats demonstrated similar effectiveness (effect size g=–0.01), in addition to 21 studies with nonequivalent treatment approaches (g=–0.06). Furthermore, in all comparisons of individual and group therapy, there were no differences in the rates of acceptance (i.e., patients in groups expressed the same level of satisfaction as those in individual therapy), remission, improvement, or premature termination. In sum, meta-analytic results demonstrate that treatment in small groups is effective compared with nonactive treatment and is equivalent to other active treatments.
A majority of studies in these meta-analyses examined group CBT approaches in the broadest sense, which included third-wave methods such as mindfulness-based therapies. Exceptions were mostly found in the efficacy research on treatments for borderline personality disorder (15), eating disorders (12), and PTSD (14), which included the use of interaction-focused and psychodynamic approaches. In addition, systemic approaches were found in studies involving multifamily groups for schizophrenia. Psychoeducational groups were also widespread and were found effective in treating schizophrenia and affective disorders (particularly bipolar disorders). A majority of studies on the efficacy of group treatments have been conducted in outpatient settings and have mainly focused on short-term groups.
Aside from the group CBT approaches, psychodynamic and group analytic approaches have the longest tradition. Nevertheless, the most recent systematic review of psychodynamic group studies (20) showed that, despite important theoretical contributions in the field, only a small number of studies reached the standards of outcome research. On the other hand, promising trends have emerged during the past decade, such as conceptual clarifications of group analytic work (21). In addition, efforts to improve research have been made. For example, Lorentzen (22) developed a transdiagnostic manual for short- and long-term group analysis that has provided the basis for studies comparing the two approaches and for detecting several moderators (23, 24). In addition, new approaches have been developed on the basis of interpersonal and psychodynamic assumptions, such as Whittingham’s (25) eight-session, manualized focused brief group therapy, which combines elements derived from process groups and attachment theory. Furthermore, Tasca et al.’s (26) integrative approach combining psychodynamic, interpersonal, and attachment theory (group psychodynamic-interpersonal psychotherapy) has led to empirical studies. Both of these approaches demonstrate that brief focused groups can be useful in the psychodynamic field and may be interpreted as a response to the overwhelming evidence for short-term group CBT. Promising psychodynamic group research can be found for mentalization-based approaches in different treatment settings and for various patient groups (27).
All studies included in the meta-analyses were RCTs implementing rigorous research designs. Although such trials generally provide less biased estimates of psychotherapy outcomes and generate substantially more replicable results than do other designs, they have been criticized for their limited external validity and absence of information on treatment mechanisms (28, 29).
An increasing number of studies have implemented rigorous study designs to test moderators of treatment efficacy in the various meta-analyses. However, no clear trends have emerged, and single moderators have proven relevant for different disorders. For example, “allegiance,” defined as the researcher’s belief in the superiority of a treatment (risk of allegiance bias lowers the effects of head-to-head comparisons in anxiety disorders) (18), group size (larger groups lead to lower effects when working with patients with borderline personality disorder) (15), and specific diagnosis (larger effects on binge eating frequency seen in binge eating disorders compared with bulimia) (12) are significant moderators. In group therapy for schizophrenia, two moderators explained variance in effect size: a higher treatment dose (i.e., increased frequency × length of sessions) produced larger effects, and advanced (i.e., doctoral-level) training of group leaders led to larger effect sizes (17). In patients with PTSD (14), gender (larger effects in women) and trauma type (smaller effects for military-sector trauma) were found to be moderators. For the other disorders, either no significant moderators were found or they were not systematically investigated (affective disorders, social anxiety, panic disorder, obsessive-compulsive disorder, substance abuse disorder) (9, 11, 13, 16, 19).
The scope of application of small group treatments has been expanded to patients with a variety of medical conditions (e.g., neurological diseases such as epilepsy and dementia). Research on group treatments for oncological patients (with a focus on breast cancer) has continued. In the 2013 chapter (5), 23 studies examining group therapy for cancer patients were summarized. These studies primarily included supportive-expressive therapy (30), CBT, and psychoeducation groups. Since then, this area of research has expanded considerably, with the largest number of group therapy studies still focusing on patients with breast cancer. Several of these studies now have long-term (up to 11 years) follow-up data available (31). Results from these studies suggest that the effects of group therapy, as demonstrated by reduced cortisol and depression, are maintained over the long term compared with outcomes among patients assigned to control conditions (31).
The predominant therapeutic approach among groups for those with general medical conditions has been CBT with a focus on stress and stress management (32), although some studies have examined psychoeducational approaches, and even fewer have focused on supportive group therapies (33). Similar to research on group therapy for mental disorders, the oncology literature shows a trend toward testing group treatments that can be classified as third-wave CBT (i.e., mindfulness-based stress reduction) (34). It has been observed that the primary outcome criteria have expanded considerably, with resilience, optimism, and posttraumatic growth investigated more often. Overall, the effects of group therapies have been relatively positive, although some studies have yielded contradictory results. The supportive-expressive groups in the tradition of Spiegel or Yalom (30, 35) have almost completely disappeared from the literature and have been replaced by third-wave approaches (e.g., mindfulness-based or acceptance and commitment treatments), which diverge from traditional CBT in that they focus more on one’s relationship with thoughts and emotions rather than on their content.
A second general medical issue that has been examined in the context of group therapies is pain. A majority of these studies have focused on chronic pain and fibromyalgia, although a minority have dealt with specific pain conditions. Nine studies on fibromyalgia published since 2013 were included in the Handbook’s most recent review (3), which tested a variety of group approaches and found relatively good effects in terms of physical function, pain-related disability, pain severity, anxiety, depression, and self-efficiency (36). Studies on chronic pain have primarily focused on coping with and reducing pain-related disability.
Overall, group studies on pain only partially confirmed the effectiveness of CBT approaches (the gold standard treatment) for pain. In any case, there are enough studies on group treatment in oncology and pain therapy to warrant a more differentiated meta-analytical consideration of the results.
The 2013 chapter on group therapy (5) summarized 250 studies concerning 12 different disorders in a systematic narrative review, despite the studies’ increasing methodological quality. In contrast, the updated review (3) refers to a total of 11 new meta-analyses, with group therapy compared with active or nonactive control conditions. All considered meta-analyses used a rigorous methodology, included RCTs only, and considered the risk of bias in the studies. In addition to the 329 studies in the meta-analyses, 40 studies on group treatments for patients with cancer or pain were included. Results from this most current review demonstrate that group treatments achieve large effects compared with nonactive treatment conditions and that the differences from other treatments, such as individual therapy, are negligible in terms of effect size. In a majority of comparisons (75%), the heterogeneity of single study effects was small, suggesting that these can be considered reliable estimates of treatment effect.
Despite these findings, existing treatment guidelines of international organizations (e.g., American Psychological Association, National Institute for Health and Care Excellence), and guidelines in German-speaking countries (Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften), recommend group therapies only in exceptional cases (37), which is both surprising and demands an explanation. One possible explanation is that group therapies have been excluded from the work of researchers who systematically summarize the evidence regarding the effects of psychotherapy.
Taken together, our current review covering about 30 years suggests that group therapy can be recommended for treating a wide range of issues. This finding is based on past comparisons of group therapy with nonactive control groups and with active treatments (Figure 2). These results need to be acknowledged and conveyed in current treatment guidelines. As Yalom and Leszcz (30) have argued, group therapy is a “triple E treatment,” meaning that it is effective compared with nonactive treatments; equivalent to other active treatments, including individual therapy; and efficient in terms of time and cost. Thus, it is worthy of being promoted by health policies.
A limitation regarding interpretation of the research findings refers to their validity for a wider range of treatments. Specifically, there is a gap between clinical-theoretical considerations of psychodynamic or group analytical approaches and specific studies in the group therapy literature. One notable exception is a Norwegian study on the empirical comparison of short- (20 sessions) and long-term (80 sessions) groups in an RCT (23). This study, based on an exemplary group analysis manual (22), suggested that the mere presence of personality pathology justifies longer-term groups (24). Presumably, the development of manuals in psychodynamic group therapy is important to stimulate further empirical research in the group-analytic context.
In addition to the development of mindfulness-based group therapies, two promising approaches have recently emerged in the interpersonal and psychodynamic context, respectively. These approaches, however, require more empirical support. Specifically, Whittingham (25) developed a manualized “ultra-short group therapy” (eight sessions of focused brief group therapy), which combines elements of process-oriented groups as defined by Yalom and Leszcz (30) and concepts of attachment theory. Tasca and colleagues (26, 38) have described group psychodynamic-interpersonal psychotherapy as an integrative group concept drawing from psychodynamic, interpersonal, and attachment-oriented approaches. The effectiveness of this therapy has been demonstrated in several studies of patients diagnosed as having disorders such as binge eating.
Another limitation relates to treatment setting, because a majority of studies on evidence-based groups have been conducted in outpatient settings with short-term groups. Controlled studies of true long-term groups are not available, except for those of the previously mentioned studies (23, 24). The last systematic summary on inpatient therapy groups was a meta-analysis published several years ago (39), which included 24 controlled studies and 46 pre-post comparisons. Results yielded a small effect for controlled studies (d=0.31) and a large effect (d=0.59) for pre-post comparisons. The largest effects were found for patients with affective disorders.
Numerous recent studies have been conducted in individual therapy to monitor the course of therapy and to help therapists identify problematic developments early in treatment. Lambert and colleagues (40) started this research, which is now widespread in many countries and shows that feedback systems can effectively detect and prevent negative developments early in treatment. In the group context, progress monitoring has been tested even less, despite its obvious use, given that group leaders are consistently tasked with monitoring the progress of several (usually eight to 10) people simultaneously.
Despite this paucity in the group literature, a wide range of methods is available to continuously and economically monitor the effects of group treatment on individuals’ symptomatology and other changes, as well as on group-specific elements (e.g., the quality of relationships between group members and member-leader). Studies (41) have tested the effects of feedback systems used to report the progress of individual group members to the group leader. In 2015, the journal Psychotherapy (42) published a special issue on progress monitoring and feedback that outlined the empirical evidence on feedback systems. Altogether, the evidence has indicated that feedback systems not only reduce problematic progressions in treatment but also can improve therapeutic outcome. This finding was reinforced by a review (43) that summarized 25 studies on feedback from patient-reported outcome measures in individual therapy.
Interest in conducting studies on using feedback in group therapy started with the findings of Chapman et al. (44), which showed that the accuracy of therapists’ prediction of change in groups corresponded little with change-related data from patients. For example, Newnham et al. (45) described the effects of feedback on treatment progress 5 days into a short-term, daily treatment. When feedback was provided, significant improvement was observed among patients whose development did not match original predictions. Additional studies (46, 47) have since shown positive effects of feedback in group therapy. In a cluster-randomized study (41) of 432 members of 58 groups at university counseling centers, progress feedback alone was tested against progress feedback plus therapeutic relationship feedback. A surprising 35% of participants produced an alert for not being on track for successful treatment outcome at least once during therapy, a result that was observed again in an archival replication study (48). The quality of the therapeutic relationship predicted improvement in outcome, and feedback appeared to reverse the course of relationship deterioration and reduce rates of treatment failure. In groups where leaders received relationship and progress feedback, there was a reduction in cases of outcome deterioration and an overall increase in outcome improvement.
Two recent meta-analyses studied the two relationship variables most frequently investigated within the group context: alliance and cohesion. Cohesion, which refers to the sense of connection or closeness among group members, is related to therapeutic outcome to the same extent reported for the therapeutic alliance in individual therapy (r=0.28) (49). In a meta-analysis (50) of 55 studies and more than 6,000 group members, a mean correlation (r=0.26) between cohesion and outcome measures was found, which can be interpreted as the mean effect. Single study results on the cohesion-outcome correlation in group therapy, however, were heterogeneous. A moderating effect was found for theoretical orientation, with the highest correlation observed for interpersonal groups, followed by psychodynamic, cognitive, supportive, and eclectic therapy groups. The cohesion-outcome association was stronger when group leaders emphasized member interaction and when groups were long lasting.
The relationship between member-leader alliance and outcomes of group therapy has been summarized in a recent meta-analysis (51). The 29 studies in this meta-analysis included 3,628 patients and yielded a significant weighted average correlation between alliance and outcome (r=0.17), which was lower compared with the correlation observed for individual treatment (r=0.28) (49). A possible explanation for this is the fact that the relationship between a patient and therapist is only one part of group therapy, but it makes up the entirety of the therapeutic relationship in individual therapy. Some moderators were observed; heterogeneity of study results could have been explained by treatment orientation (lower correlation for CBT than for other group treatments) and the reporting perspective (higher correlation for patient-reported than for mixed or observer-reported alliance).
In addition to cohesion and alliance, patient characteristics may influence group therapy outcomes. Specifically, the influence of attachment characteristics on treatment effects has been examined (52). Over the past decade, numerous studies have shown that positive changes in attachment characteristics do indeed contribute to improvements in interpersonal problems and in other psychological symptoms (53). Analogous findings have been reported from social and organizational psychology. Based on these results, it has been postulated that “repeated interactions with responsive and supportive leaders and cohesive groups beneficially alter a person’s attachment patterns and psychological functioning” (54). In the context of attachment research, other methodological approaches have been tested, such as the actor-partner independence model (55) and attachment heterogeneity in groups (56). Overall, the research shows high relevance for attachment characteristics in group treatment, a finding that should encourage group leaders to attend to the influence of attachment goals on group members’ behavior and the impact of attachment characteristics on members’ willingness to engage with and stay in the group. Attachment characteristics may also moderate the relationship between group cohesion and member outcomes and should therefore be considered during group composition and selection of members. Another area for future development, consistent with those occurring in individual psychotherapy, includes development of Internet-based group treatments relying on both asynchronous (i.e., Internet forum providing contact to a therapist) and synchronous (i.e., real time) online contact. In this regard, the field has made considerable progress in the last years, reflecting new technologies that allow such interventions to reach a wider range of patients than face-to-face settings.
Overall, the amount and diversity of research on group psychotherapy have increased significantly during the past decade. Despite demonstrating good to excellent efficacy, group therapy is rarely recommended by clinical guidelines, possibly because of delays in consideration of new results. Numerous studies on specific predictors and process factors have demonstrated that attachment characteristics and therapeutic relationships in groups (i.e., alliance and cohesion) are relevant predictors of treatment outcomes. These findings have been consistent for different groups and for a wide range of formal change theories, leading to the recommendation for consideration of these factors in practice.
Research on attachment issues in group psychotherapy and on the use of Internet-based groups is promising. Together with group therapy’s favorable cost-benefit ratio, the available evidence should encourage psychotherapists to increase the use of group therapy and to acquire competence in this specialty if they do not already have it.